Understanding Pancreatic Tumor Symptoms
Introduction to Pancreatic Cancer
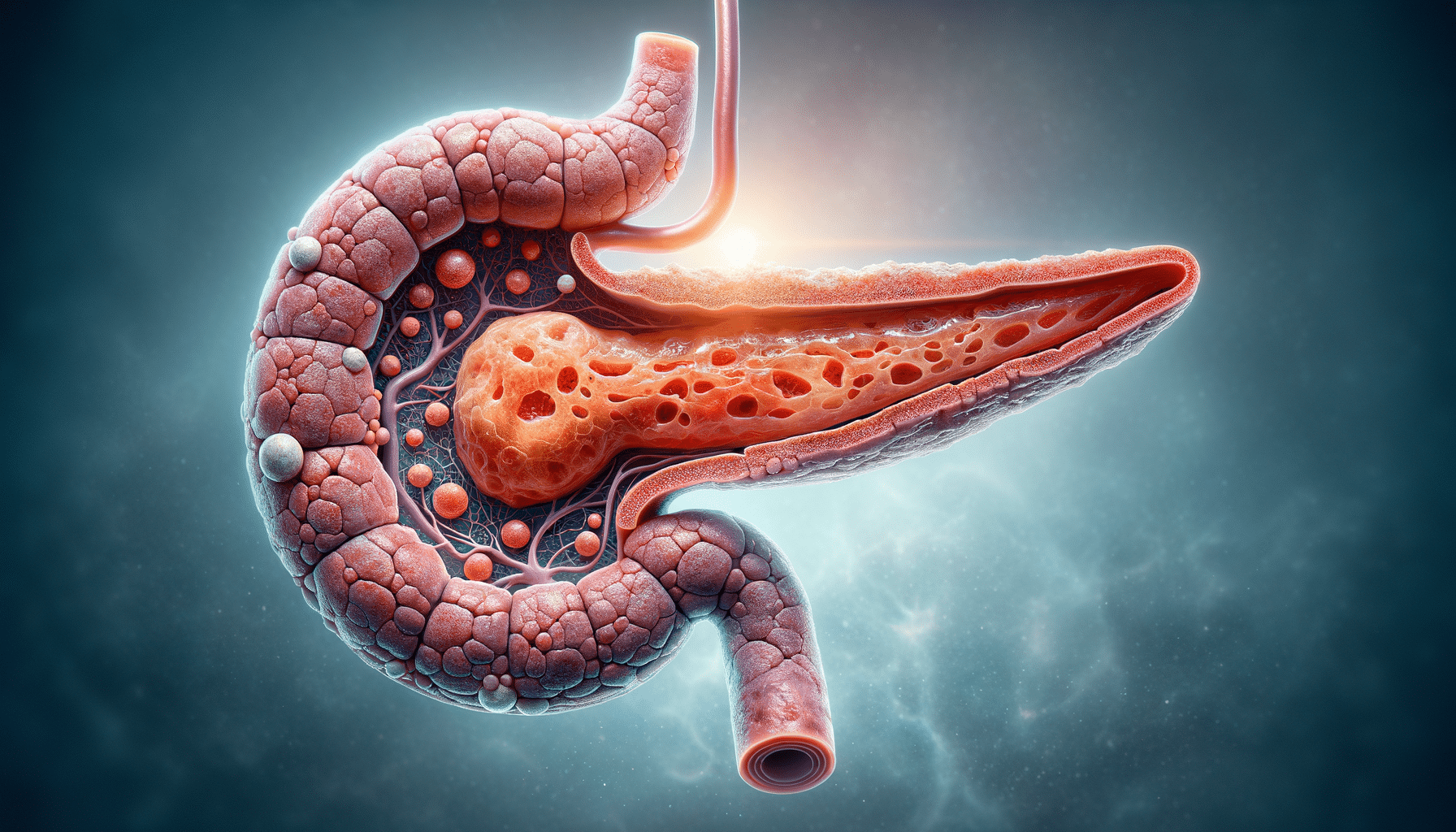
Pancreatic cancer is a formidable disease that affects thousands of individuals worldwide each year. It is a condition where malignant cells form in the tissues of the pancreas, an organ located behind the stomach that plays a critical role in digestion and blood sugar regulation. Understanding the symptoms and early signs of pancreatic cancer is crucial for timely diagnosis and treatment, which can significantly impact the prognosis and quality of life for patients.
The importance of recognizing pancreatic cancer symptoms cannot be overstated. Early detection can lead to more effective treatment options and improved survival rates. However, the symptoms of pancreatic cancer are often subtle and can be easily mistaken for other less severe conditions, making awareness and education vital components in the fight against this disease.
Common Symptoms of Pancreatic Cancer
Pancreatic cancer symptoms can vary depending on the type and stage of the cancer. Some of the most common symptoms include:
- Jaundice: A yellowing of the skin and eyes caused by the buildup of bilirubin, a substance produced by the liver.
- Abdominal pain: Often described as a dull ache in the upper abdomen that may radiate to the back.
- Unexplained weight loss: Sudden and unintended weight loss can be an early sign of pancreatic cancer.
- Loss of appetite: A decrease in appetite or feeling full quickly after eating small amounts.
- Changes in stool: Stools may become greasy or float due to the pancreas not producing enough enzymes to digest fat.
These symptoms can also be indicative of other medical conditions, which is why it is important to consult a healthcare professional if they persist. Early intervention can lead to a more favorable outcome.
Risk Factors and Causes
Understanding the risk factors associated with pancreatic cancer can help in assessing individual risk and taking preventive measures. Some of the key risk factors include:
- Smoking: Cigarette smoking is one of the most significant risk factors for pancreatic cancer.
- Family history: A family history of pancreatic cancer can increase an individual’s risk of developing the disease.
- Chronic pancreatitis: Long-term inflammation of the pancreas is linked to an increased risk of pancreatic cancer.
- Diabetes: There is a correlation between diabetes and pancreatic cancer, though the exact relationship is not fully understood.
- Age: The risk of pancreatic cancer increases with age, with most cases occurring in individuals over 60.
While some risk factors such as age and family history cannot be changed, lifestyle modifications like quitting smoking and maintaining a healthy weight can help reduce the risk.
Diagnosis and Treatment Options
Diagnosing pancreatic cancer typically involves a combination of imaging tests, blood tests, and biopsy procedures. Imaging tests such as CT scans, MRI, and endoscopic ultrasound can help visualize the pancreas and identify any abnormal growths. Blood tests may include checking for tumor markers such as CA 19-9, although these are not definitive for diagnosis.
Once diagnosed, treatment options for pancreatic cancer depend on the stage and location of the tumor, as well as the patient’s overall health. Common treatment methods include:
- Surgery: Procedures like the Whipple procedure can remove tumors in the pancreas.
- Chemotherapy: Drugs are used to kill cancer cells or stop them from growing.
- Radiation therapy: High-energy rays are used to target and destroy cancer cells.
- Targeted therapy: Drugs that specifically target cancer cell growth mechanisms.
Early-stage pancreatic cancer may be treated with surgery, while advanced cases often require a combination of chemotherapy and radiation therapy. The treatment plan is tailored to each patient’s specific needs and circumstances.
Living with Pancreatic Cancer
Receiving a diagnosis of pancreatic cancer can be overwhelming, and living with the disease requires a comprehensive approach that includes medical treatment, emotional support, and lifestyle changes. Patients are encouraged to work closely with their healthcare team to manage symptoms and side effects of treatment.
Support groups and counseling can provide emotional and psychological support, helping patients and their families cope with the challenges of the disease. Nutrition and exercise are also important aspects of living with pancreatic cancer, as they can help improve overall health and well-being.
Advancements in research continue to offer hope for new treatments and improved outcomes for pancreatic cancer patients. Staying informed and actively participating in one’s care can empower patients to navigate their journey with confidence and resilience.


