Comprendere i sintomi del tumore al pancreas
Understanding Pancreatic Cancer
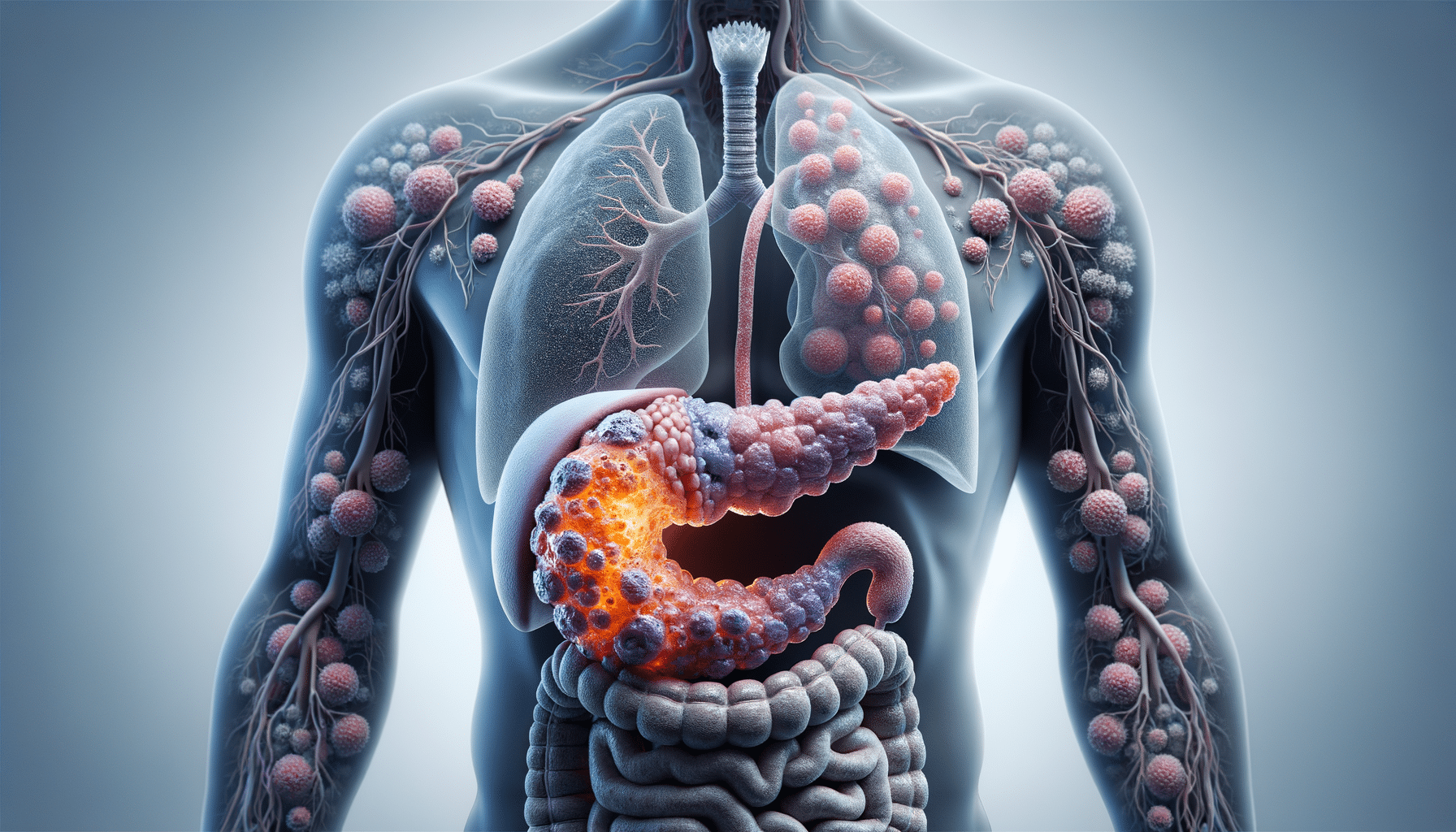
Pancreatic cancer is a formidable adversary in the realm of health, characterized by its stealthy progression and often late diagnosis. The pancreas, a vital organ nestled in the abdomen, plays a crucial role in digestion and blood sugar regulation. Unfortunately, when cancer strikes this organ, it often goes unnoticed until it reaches an advanced stage. Understanding pancreatic cancer involves delving into its anatomy, function, and the nature of cancerous growths that can develop within it.
Pancreatic cancer typically falls into two categories: exocrine tumors, which are the most common, and endocrine tumors, which are rarer. Exocrine tumors, such as adenocarcinomas, arise from the ducts of the pancreas and are known for their aggressive nature. Endocrine tumors, on the other hand, originate from hormone-producing cells and tend to grow more slowly. Recognizing the distinction between these types is crucial in determining the appropriate treatment approach.
Several risk factors contribute to the development of pancreatic cancer. These include age, smoking, obesity, chronic pancreatitis, and a family history of the disease. While some risk factors, like age, are beyond our control, lifestyle changes such as quitting smoking and maintaining a healthy weight can reduce the likelihood of developing this type of cancer.
Signs and Symptoms
One of the most challenging aspects of pancreatic cancer is its tendency to remain asymptomatic until it has progressed significantly. Early detection is often hampered by the subtlety of its symptoms, which can easily be mistaken for less serious conditions. However, being aware of potential warning signs can make a difference in seeking timely medical attention.
Common symptoms of pancreatic cancer include jaundice, unexplained weight loss, abdominal pain, and changes in stool. Jaundice, characterized by yellowing of the skin and eyes, occurs when a tumor obstructs the bile duct. This blockage leads to a buildup of bilirubin in the body. Abdominal pain, often radiating to the back, can be persistent and severe, while unexplained weight loss and changes in appetite may signal underlying issues.
It’s essential to note that these symptoms are not exclusive to pancreatic cancer and can be associated with various other conditions. However, if they persist or worsen, consulting a healthcare professional is advisable. Early detection and diagnosis can significantly influence treatment options and outcomes.
Diagnosis and Staging
The diagnosis of pancreatic cancer involves a combination of imaging tests, biopsies, and blood tests. Imaging techniques such as CT scans, MRI, and endoscopic ultrasound provide detailed views of the pancreas and surrounding structures, aiding in the identification of tumors. A biopsy, where a small tissue sample is taken for analysis, confirms the presence of cancer cells.
Once diagnosed, staging the cancer is crucial for determining the extent of its spread and guiding treatment decisions. Pancreatic cancer is staged using the TNM system, which considers the size of the tumor (T), the involvement of lymph nodes (N), and the presence of metastasis (M). Stages range from I to IV, with Stage I indicating localized cancer and Stage IV representing advanced cancer with distant spread.
Understanding the stage of pancreatic cancer is vital for tailoring treatment plans. Early-stage cancers may be amenable to surgical resection, while advanced stages often require a combination of chemotherapy, radiation, and supportive care to manage symptoms and improve quality of life.
Treatment Options
Treatment for pancreatic cancer varies depending on the stage at diagnosis and the patient’s overall health. Surgery, chemotherapy, radiation therapy, and targeted therapies are among the primary treatment modalities. Each approach has its benefits and limitations, and treatment plans are often individualized to meet the patient’s specific needs.
Surgical options, such as the Whipple procedure, aim to remove the tumor and affected tissues. This is generally considered when the cancer is localized and operable. Chemotherapy uses drugs to target and destroy cancer cells, often used in conjunction with surgery or as a standalone treatment in advanced cases. Radiation therapy employs high-energy rays to shrink tumors and alleviate symptoms.
In recent years, targeted therapies and immunotherapy have emerged as promising avenues for treatment. These approaches focus on specific genetic mutations or enhance the body’s immune response to fight cancer cells more effectively. While these treatments offer hope, they are typically used in conjunction with traditional therapies.
Living with Pancreatic Cancer
Living with pancreatic cancer presents numerous challenges, both physically and emotionally. Patients often face a complex journey that requires resilience and support. Managing symptoms, maintaining nutrition, and addressing the emotional toll are integral parts of navigating life with this disease.
Supportive care plays a crucial role in enhancing quality of life. This includes pain management, nutritional support, and psychological counseling. Many patients benefit from joining support groups where they can connect with others facing similar challenges. Sharing experiences and coping strategies can provide comfort and encouragement.
It’s important for patients and their families to maintain open communication with healthcare providers. Discussing treatment goals, potential side effects, and palliative care options ensures that care aligns with the patient’s values and preferences. While pancreatic cancer is a daunting diagnosis, a comprehensive approach that addresses medical, emotional, and social aspects can improve the journey for patients and their loved ones.


